I am becoming increasingly convinced the communication gap between veterinarians and clients is the number one problem we’ve failed to solve. We’re just not on the same page a lot of the time, it seems, and it makes me sad. I can’t read a single article online without coming across “veterinarians are money grubbing pigs that suck” (true blog title) and someone else saying “if you can’t afford x/y/z/q you shouldn’t have gotten a pet, jerk.” I feel as though this is perhaps a bit extreme, but it’s what happens when we don’t work together to identify our goals.
Common Fallacies of Bad Client Interactions
(In just as many cases, the vet on the left is an associate up to his or her ears in student debt and just trying to make it through the day without getting yelled at one more time, and the client on the right is a stressed out single parent who just spent a grand fixing her car.)
Much of this angst comes from the pervasive assumption that in all cases we will do everything we can medically, no matter what, which was fine a while back when “everything” meant “antibiotics” but as veterinary medicine has advanced, has come to mean “MRI, spinal tap, radiation.”
This assumption, of course, carries over from human medicine: if you’ve got the insurance, you’re getting the treatment. Everyone’s happy, right? Right?
Not so much. Satisfaction with a medical course of action relies on multiple factors.
Sometimes getting to “Everyone Happy” (Square B) is impossible. D’s not so bad either, but A and C are no-fly zones.
Human Medicine Satisfaction
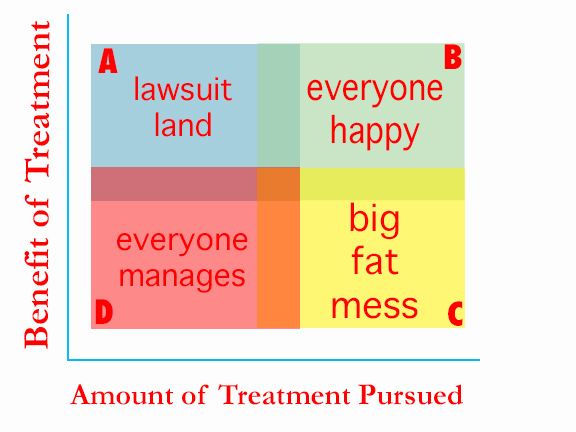
I would argue that satisfaction with outcomes is directly correlated to the balance between the amount of treatment pursued, and its benefit.
So really, the goal here isn’t to push everyone towards the far extremes of treatment; it’s about getting to that center line of balance. In human medicine this change is slowly creaking along with things like hospice care, which moves people from C to D in low treatment benefit situations, and increased access to insurance coverage, which moves you from A to B in high benefit situations. With Mom, we were squarely in the D category, and while we’re not HAPPY, it’s a hell of a lot better than if we had treated her to death.
Make sense?
So how does this apply to veterinary medicine? It’s similar, except we tend to find ourselves walking a line most strongly related to finances.
The Veterinary Experience
There’s a whole lot of people in square C these days, who spent more than they really had on treatments they weren’t sure they wanted, because they felt like they had to, and when things go downhill as they often do with very ill pets, people can end up really, really disillusioned with the profession.
Now, since we have no ability to magically divine which people are up for specialty treatment and which people are not, we always offer all the options to clients- as we should. There are people who spend thousands, lose their pet, and are still ok with the outcome- but they were also very clear on the risks and made an informed decision. Many clients, it seems, feel as if they are not.
So what do we do to improve outcomes? In my experience, the best way to move the dial from A to B is pet insurance, at least for emergency situations. There are few situations more likely to prompt a Facebook mob than a pet who died a preventable death because the owner couldn’t afford treatment and the ER vet wouldn’t do the treatment for free- nor should they. Owners need to shoulder some of the responsibility here of financial preparation, and if they refuse to take even basic steps to be prepared, maybe they really are a crappy client.
And conversely, moving the dial from C to D involves good veterinary communication, and a willingness to understand that lots of factors go into the decision about whether or not to seek treatment. If a veterinarian talks a senior on a fixed income into a kidney transplant for a 15 year old cat in renal failure, after she expressed concern about paying her rent for the month and her own upcoming surgery- maybe they really are a money grubbing vet.
But I like to give everyone the benefit of the doubt. Clients and vets both have work to do here. And I believe with all of my heart that the better we get about empowering clients to make informed decisions, the more that will carry over into human medicine- which is a wonderful thing.
I realize this is a vastly oversimplified explanation of some really complicated issues, but hey, we have to start somewhere. Whatever it is we’re doing now sure doesn’t seem to be working too well.






I suspect that the decisions people make about their pets’ health is strongly related to their expectations about their own health and treatment. I’ve certainly seen it in my own family.
I’m skeptical about intensive medical treatment for myself and my primary goal is to have good overall health and a high quality of life. I want the same thing for my pets.
My husband is a childhood cancer survivor whose family has chronic medical problems like diabetes and COPD. He’s more interested in intense medical intervention for himself and our pets.
I wonder if a few questions on a first visit questionnaire about general attitudes toward medical interventions would be a helpful tool for starting conversations?
And, of course, a little empathy goes a long way.
I feel as you do Pamela. My end of life arrangements are for pain relief and some peace and quiet. My doctor and I talked about it so we both know what the other thinks. I did the same with my vet. Death is a part of living in all of creation. Our society is not always comfortable with that reality.
I absolutely agree. The overlap between our own experiences and the choices we make for our pets is much stronger than we realize, I think. Both directions.
I’m so fortunate living in small town Iowa and having my grumble of pugs (5) that I have found a vet only 6 miles away that also loves pugs. She has her own and is well versed in their care and the do’s and don’ts of medications unique to the breed. She is well aware of my fierce love of all of my critters both past and present and treats me like an educated dog mom. She remembers the names of past pets without consulting a chart. She allows me to carry a cash balance forward so that if we have an emergency we can still eat that month. But doesn’t take advantage of that. She will advise me if a treatment not beneficial for my pet. My vet is a Godsend!!
When the animal is really sick and euthanasia is a realistic option, I wish they would tell me that, rather than send us home with medicine and subq fluids and needles and sometimes insulin and all those other treatments, when in reality, it woud be kinder to just let the pet go. The last couple of times, I have had to ask if euthanasia is appropriate at this point and they have always said yes. Why do they make me ask? Why not suggest it as a possibility? They make me feel like an irresponsible pet owner if I don’t drag the pet’s life out even though the quality is gone.